Forensic Mental Health Services for Older People
Forensic mental health services provide care for people who are in the criminal justice system and mentally unwell. The service includes treatment, rehabilitation and follow-up care for both mental and physical illnesses.1
This post looks at some of the specific challenges that older people receiving forensic mental healthcare face. We also discuss how a specialist mental health bed can help to address some of these.
Introduction
Around 20% of the UK forensic mental health inpatient population is aged 50 or over.2 However, this is likely to increase as the overall population continues to grow in both numbers and as a percentage.3 For example, between 2013 and 2019 in Scotland, the number of forensic inpatients aged over age 65 grew by 50%.4
Many older people receiving forensic mental healthcare have a complex mix of physical, psychological and cognitive needs, different from those of younger people.5 For example, previous research has shown that older people are more likely to be diagnosed with depression, delusional disorder and dementia.6 Additionally, poor physical health has been found to be more common.7
Older forensic mental healthcare patients in England – 2022 study
The authors of this study identified that the health needs of older forensic mental health patients were not well understood. Therefore, they recruited 37 patients aged 55 or over to participate, from a mixture of low, medium and high security hospitals and community care.2 The participants completed questionnaires, covering their:
- Physical health
- Mental well-being
- Cognitive ability
- Quality of life
Study Results
The study found that the patients had complex health needs. Of the participants, 92% were male, with a mean age of 60 years. The median length of stay in the current institution was 1,404 days (45 months).
The most common physical health problems were:
- Diabetes (48.7%)
- Cardiovascular/circulatory disease (37.8%)
- High cholesterol (18.9%)
- Chronic obstructive pulmonary disease (16.2%)
- Visual impairment (13.5%)
On average, patients were prescribed 7.6 medications, many of which had significant side effects.
The most common mental health diagnoses were:
- Schizophrenia, schizotypal and delusional disorders (59.5%)
- Personality disorders (40.5%)
- Mood (affective) disorders (16.2%)
In addition, possible cognitive impairment was identified in 65% of participants.
Participants who were able to carry out everyday activities scored higher in the quality of life assessment than those who were less able.
How Can a Bed Help?
The results of the above study and other published research demonstrate that this cohort has a complex mixture of physical and mental health problems.
For individuals in poor physical health who are also at risk of harming themselves or others, an electric profiling bed may be able to benefit them physically. Specifically, it can help with easier/earlier mobilisation, upright positioning and reducing the risk of falls. In turn, this can help to reduce deconditioning and frailty.
Having said this, using a standard med/surg hospital bed for these patients has several major risks associated, including:
- Ligature risks, with numerous potential attachment or anchor points on the bed.
- The ability to remove parts of the bed which can be used as a weapon.
- A non-removable electric handset, where unauthorised use could result in serious injury.
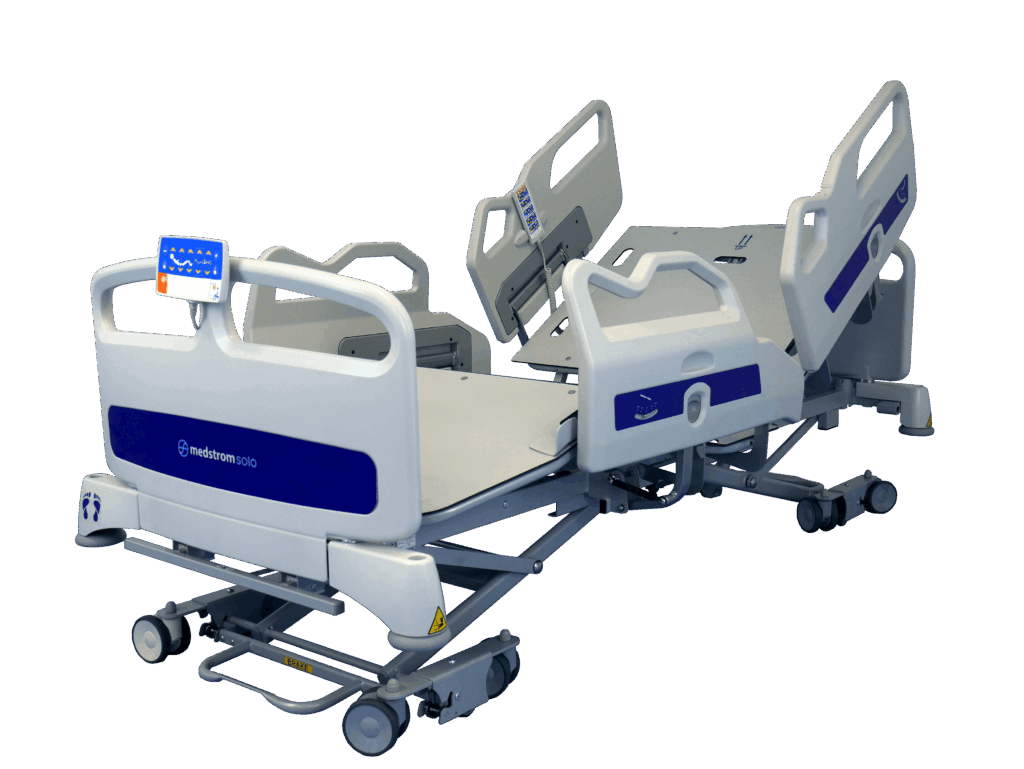
Medstrom SoloMH Bed

To address these challenges, the Medstrom SoloMH mental health bed has been designed in collaboration with key opinion leaders within the mental health environment. Specifically, it has several adaptations that optimise safety and provide enhanced protection:
- A remote, wireless handset, removable mains cable, covered wires, anti-intrusion plates and a design which minimises anchor points all help to reduce ligature risks.
- Fixed sleep deck panels and head/foot ends prevent removal.
- Fixed side panels prevent removal, and at the bed’s lowest height they rest on the floor, to stop entrapment underneath.
- Many components are made with highly durable and shatterproof polycarbonate.
Clinical benefits include:
An ultra-low height of 19cm helps to reduce the risk of injury from falls, and means almost all patients who are able can mobilise safely from the bed.
- A unique custom mobilisation height, set for each patient, means the patient always starts to mobilise from an optimum position, with their feet flat on the floor.8
- Full electric profiling and a one button cardiac chair can help with in-bed mobilisation and optimising positioning for clinical needs.
- The unique 2D elliptical backrest movement adds 23cm to the platform length. This mimics spine elongation when a person goes from lying to sitting, preventing heel travel and the associated shear and friction.
For more information on the SoloMH mental health bed please contact us, and one of our qualified, experienced Clinical Advisors will get in touch with you.
References
-
Rapid review into data on mental health inpatient settings: final report and recommendations (2024). Department of Health and Social Care. Available at: Rapid review into data on mental health inpatient settings: final report and recommendations – GOV.UK (www.gov.uk)
-
Tomlin J, Walker K, Yates J, Dening T, Völlm B, Griffiths C. Older forensic mental healthcare patients in England: demographics, physical health, mental wellbeing, cognitive ability and quality of life. NIHR Open Res. 2022;2:9. Published 2022 Jun 22. doi:10.3310/nihropenres.13248.2
-
Profile of the older population living in England and Wales in 2021 and changes since 2011 (2023). ONS. Available at: Profile of the older population living in England and Wales in 2021 and changes since 2011 – Office for National Statistics (ons.gov.uk)
-
Independent Review into the Delivery of Forensic Mental Health Services (2021). Scottish Government. Available at: Independent Forensic Mental Health Review : final report (www.gov.scot)
-
Natarajan M, Mulvana S. New horizons: Forensic mental health services for older people. BJPsych Advances. 2017;23(1):44–53. 10.1192/apt.bp.113.012021
-
Coid J, Fazel S, Kahtan N: Elderly patients admitted to secure forensic psychiatry services. J Forensic Psychiatr. 2002;13(2):416–427. 10.1080/09585180210154470
-
di Lorito C, Völlm B, Dening T: The characteristics and needs of older forensic psychiatric patients: a cross-sectional study in secure units within one UK regional service. J Foren Psychi Psych. 2019;30(6):975–992. 10.1080/14789949.2019.1659390
-
Martindale D (2021). Calculating bed height for hospital patients using popliteal measurement. Nursing Times [online]; 117: 10.