Are Pressure Ulcers Avoidable?
Firstly, it should be remembered that all patients are potentially at risk of developing a pressure ulcer1. Therefore, a risk assessment should form the basis for planning, implementing, and evaluating preventive care for all patients and why frameworks such as aSSKINg, forms part of the new core curriculum for pressure ulcer education2. This basis for decision making, should be re-assessed, based on the patient’s overall condition and upon any clinical changes3,4.
NICE (2014) state that some patients are more at risk than others. This includes:
- significantly limited mobility (for example, people with a spinal cord injury)
- significant loss of sensation
- a previous or current pressure ulcer
- nutritional deficiency
- the inability to reposition themselves
- significant cognitive impairment
The above subset of patients are all at a higher risk and steps to reduce occurrence of pressure damage should be taken, as directed by a risk assessment framework and clinician’s own decision. These steps will involve multifactorial care approaches such as increased repositioning, nutritional referral and proactive planning of equipment needs.
Terminology around pressure ulcers being preventable or avoidable are used interchangeably. Stop the Pressure and NHS Improvement state “many pressure ulcers are preventable”5. NHS England (2019)6 state, “many pressure ulcers are avoidable if simple knowledge is provided and preventative best practice is followed.” NICE suggest they are “largely preventable however it is accepted that some cannot be avoided for example due to compliance with prevention strategies, end of life care or for other issues.”7.
Terminology surrounding avoidable and unavoidable comes historically where an omission meant one of the following did not occur:
- Evaluate the person’s clinical condition, and pressure ulcer risk factors
- Plan and implement interventions consistent with the person’s needs and goals, and with recognised standards of practice
- Monitor and evaluate the impact of the interventions; or
- Revise the interventions as appropriate
An “unavoidable” pressure ulcer occurred where the above criteria could be evidenced to have been achieved and the pressure ulcer still occurred8.
NHS Improvement (2018b)9, stated that the use of terms “avoidable” and “unavoidable” pressure ulcers should not be used in the Department of Health and Social Care’s definition of a pressure ulcer. This could be due to concerns, voiced by White et al (2014)8, of the ramifications of such terminology. For example, would this have consequences or effect on-going patient care?
In 1998 Hibbs10 hypothesised about previous work “I was convinced then and I still am that 95% of all pressure sores could be prevented”, this figure has persisted but is debated in more recent studies. A study undertaken in the Midlands in 2012, put this figure at 57% of pressure ulcers were avoidable.
Despite any debate on terminology and following NHS Improvements guidance, there should be no use of “avoidable” and “unavoidable” pressure ulcers. Ethically and morally, the goal of care must be to do all that is possible to prevent the development of a pressure ulcer8.
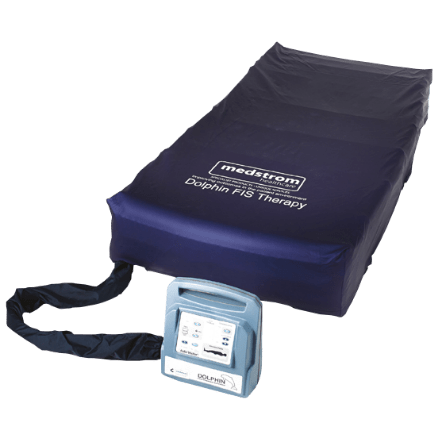
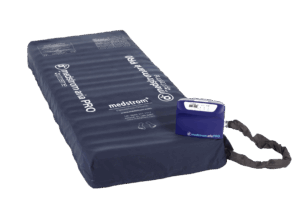
At Medstrom, we are committed to providing innovative, clinically effective and cost-effective support surfaces for the treatment of all categories of pressure ulcer, including those very complex patients for whom traditional dynamic surfaces are not sufficient.
Download Our Pressure Ulcer Guide
Learn More About Pressure Ulcers Here